בבא קמא לה, א
ההוא תורא דהוה בי רב פפא דהוה כיבין ליה חינכיה עייל ופתקיה לנזייתא ושתי שיכרא ואיתסי
There was an ox in the house of Rav Pappa that had a toothache. It went inside, pushed the cover off a beer barrel, drank the beer, and was healed.
Descartes on Animal Pain
The silly notion that animals do not feel pain is widely thought to have originated with the French philosopher Rene Descartes (1596-1650). "They eat without pleasure, cry without pain, grow without knowing it; they desire nothing, fear nothing, know nothing". While these words were those a student of Descartes, the contemporary philosopher Peter Harrison notes that they are generally thought to capture the essence of Descartes' view of animals. "The father of modern philosophy" continues Harrison, "is credited with the opinion that animals are non-sentient automata, an opinion for which over the centuries he has been ridiculed and vilified."
“To be able to believe that a dog with a broken paw is not really in pain when it whimpers is a quite extraordinary achievement, even for a philosopher.”
Scientists Ignoring Animal Pain
Vivisection of a dog. From J. Walaeus. Epistola Prima de Motu Chyli et Sanguinis (1647).
The debate as to Descartes' true view is fascinating, but need not detain us. What is certain is that the pain that animals undoubtedly feel was either denied as existing, or overlooked for centuries by scientists. Animals were used for experiments of the most horrendous kind in the names of science, even when the pain was evident to those who were causing it. Here, for example, is the French physiologist Claude Bernard (d. 1878), who felt that without vivisection, 'neither physiology not scientific medicine is possible':
A physiologist is not a man of fashion, he is a man of science, absorbed by the scientific idea where he pursues: he no-longer hears the cry of animals, he no-longer sees the blood that flows, he sees only his idea...no anatomist feels himself in a horrible slaughter house; under the influence of a scientific idea, he delightfully follows a nervous filament through stinking livid flesh, which to any other man would be an object of disgust and slaughter.
“It is sometimes said that people in the seventeenth century had no motion of cruelty to animals and Descartes even argued that animals are mere machines, incapable of feeling pain. It is also said there was so much cruel treatment of one human being by another in the seventeenth century that what was done by the vivisectionists to animals would scarcely have seemed horrendous. ”
Do Fish Feel Pain? - Yes!
The tropical Zebrafish grow to about 2.5 inches in length. And they don't like pain.
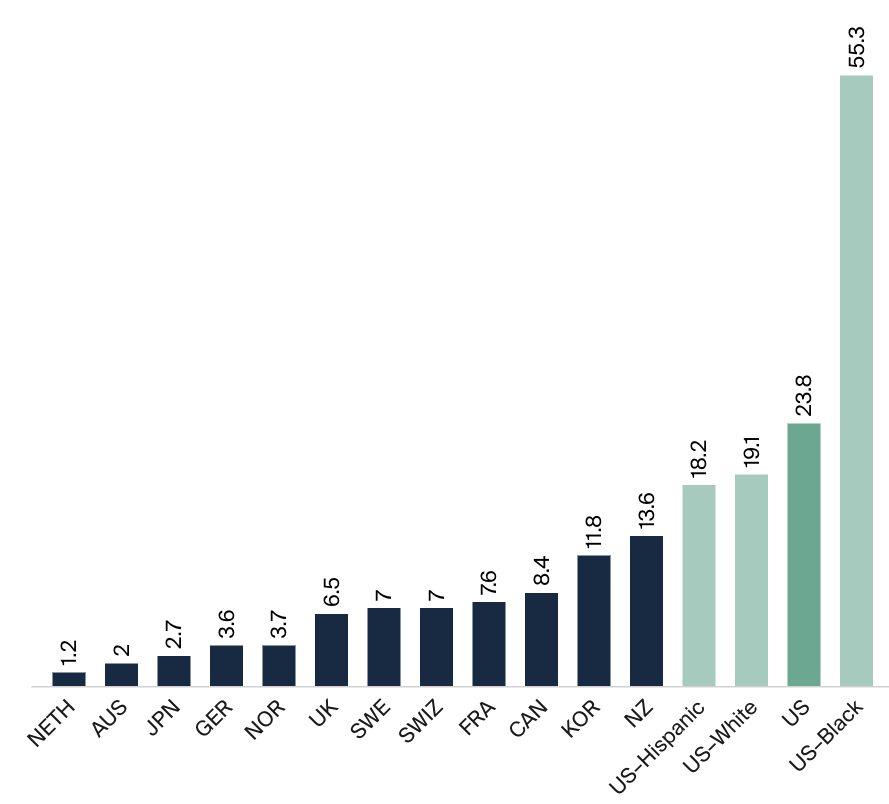
Rav Pappa's ox sought out pain relief from beer, but recent evidence has shown that it's not just oxen who like to have their pain relieved. So do fish. In a paper in the The Journal of Consciousness Studies, Lynn Sneddon demonstrated that not only can fish feel pain, but that they are willing to pay a cost to get pain relief. Zebrafish, like humans, prefer an interesting environment to a boring one. When given a choice, these fish swim in an enriched tank with vegetation and objects to explore, rather than in one that is bare. With me so far? OK. Next, Sneddon, from the University of Liverpool in the UK, injected the tails of the zebrafish with acetic acid, which no doubt annoyed them, but did not cause any change in their preference for the interesting tank over the one that was bare. Finally, she injected the fish with acetic acid, but added a painkiller into the water of the bare tank. This time, the fish chose to swim into the bare but drug filled tank. Fish who were injected with saline as a control remained in the enriched tank and did not swim into the drug enhanced bare tank. The conclusion: zebrafish are willing to pay a cost in return for getting relief from their pain. Similar observations have been made in rodents too; when in pain, they will self administer analgesics, preferring to drink analgesic dosed water or eat dosed food when presented with a choice.
Defining Animal Pain
In the scientific world there was - and perhaps still is - a debate about the nature of pain that animals may feel. Sneddon, the fish physiologist, wrote that if we are to conclude that animals experience pain in a way similar to humans, then (1) "animals should have the apparatus to detect and process pain; (2) pain should result in adverse changes in behavior and physiology; and (3) analgesics (painkillers) should reduce these responses..." Thanks to advances in microscopy and physiology, today we know that animals have many of the anatomical features (like nerves that transmit the pain stimulus) needed to process pain.
The Ox of the House of Rav Pappa
Rav Pappa's ox demonstrated the second and third of Sneddon's features: pain changed the behavior of the ox (off it trotted to find pain relief ), and analgesia, (in this case beer) indeed reduced the pain response. Of course we are left wondering how it was known that the ox of the house of Rav Pappa specifically had a toothache, (and not say sinusitis or a bad migraine), but based on what we know about the ways in which fish and rodents will seek out an environment in which painkillers are available, the story is no where near as fanciful as we might suspect.
קיצור שולחן ערוך - קצא
אָסוּר מִן הַתּוֹרָה לְצַעֵר כָּל בַּעַל חָי. וְאַדְּרַבָּא, חַיָב לְהַצִּיל כָּל בַּעַל-חַי מִצַּעַר
It is forbidden to cause pain to any living creature. In fact a person is required to save any living creature from pain...(Abbreviated Code of Jewish Law by Shlomo Ganzfreid, 1864).